Body mass index (BMI) & ideal weight in Orthopaedics
BMI & ideal weight are two simple and essential tools for evaluating an individual's physical condition. These indexes assume importance in the field of Orthopaedics as independent factors for musculoskeletal injuries prevention and with regards to the outcomes of orthopaedic surgical procedures.
Table of contents
What is BMI? Why does it matter?
Ο Δείκτης Μάζας Σώματος υπολογίζεται διαιρώντας το βάρος (σε κιλά) με το τετράγωνο του ύψους (σε μέτρα). Παρόλο που δεν λαμβάνει υπόψη τη μυϊκή μάζα ή την κατανομή του λίπους, αποτελεί έναν γενικό δείκτη της σχέσης βάρους/ύψους. Οι τιμές του κατηγοριοποιούνται ως εξής:
- Κάτω από 18,5: Ελλιποβαρής
- 18,5 – 24,9: Φυσιολογικό βάρος
- 25 – 29,9: Υπέρβαρος
- 30 και άνω: Παχυσαρκία

Η διατήρηση ενός φυσιολογικού BMI δεν είναι απλώς θέμα εμφάνισης. Από ορθοπαιδική σκοπιά, είναι ζωτικής σημασίας για τη μακροχρόνια υγεία των αρθρώσεων και των οστών.
Ideal weight as point of reference
Το Ιδανικό Βάρος υπολογίζεται με βάση το φύλο και το ύψος του ατόμου, χρησιμοποιώντας τύπους όπως ο τύπος Devine. Αν και πρόκειται για προσέγγιση, προσφέρει ένα εύχρηστο σημείο αναφοράς για να θέσει κανείς ρεαλιστικούς στόχους σωματικής υγείας.

How is MSK health related to these indexes?
1. Επιβάρυνση των αρθρώσεων
Οι αρθρώσεις, ειδικά των κάτω άκρων – όπως τα γόνατα, τα ισχία και η ποδοκνημική – δέχονται μεγάλη επιβάρυνση σε κάθε βήμα. Ένα επιπλέον κιλό σωματικού βάρους μεταφράζεται σε πολλαπλάσια καταπόνησηγια τις αρθρώσεις κατά τη διάρκεια της βάδισης ή της άσκησης. Αυτό επιταχύνει τη φθορά του αρθρικού χόνδρου και μπορεί να οδηγήσει σε πρώιμη οστεοαρθρίτιδα.
2. Ανάρρωση μετά από χειρουργική επέμβαση
Μετά από επεμβάσεις όπως η αρθροσκόπηση ώμου ή γόνατος, η αντικατάσταση ισχίου ή γόνατος ή άλλες ορθοπαιδικές επεμβάσεις, ο έλεγχος του σωματικού βάρους είναι κρίσιμος για την επιτυχή αποκατάσταση. Ασθενείς με αυξημένο ΔΜΣ παρουσιάζουν μεγαλύτερα ποσοστά επιπλοκών, δυσκολία στην κινητοποίηση και μεγαλύτερη φθορά στα εμφυτεύματα.
3. Μυοσκελετική υποστήριξη και μυϊκή ισορροπία
Τα άτομα με πολύ χαμηλό βάρος μπορεί να έχουν χαμηλή μυϊκή μάζα και μειωμένη οστική πυκνότητα, αυξάνοντας τον κίνδυνο καταγμάτων ή προβλημάτων στάσης. Αυτό είναι ιδιαίτερα σημαντικό για ηλικιωμένους και μετεγχειρητικούς ασθενείς.
Who should monitor BMI & ideal weight?
✅ Ασθενείς με χρόνιους πόνους
Άτομα με χρόνιο πόνο στη μέση, στα ισχία ή στα γόνατα μπορούν να ωφεληθούν ιδιαίτερα από την απώλεια περιττού βάρους. Ακόμη και 5-10% μείωση του σωματικού βάρους μπορεί να μειώσει σημαντικά την ένταση του πόνου και να βελτιώσει την κινητικότητα.
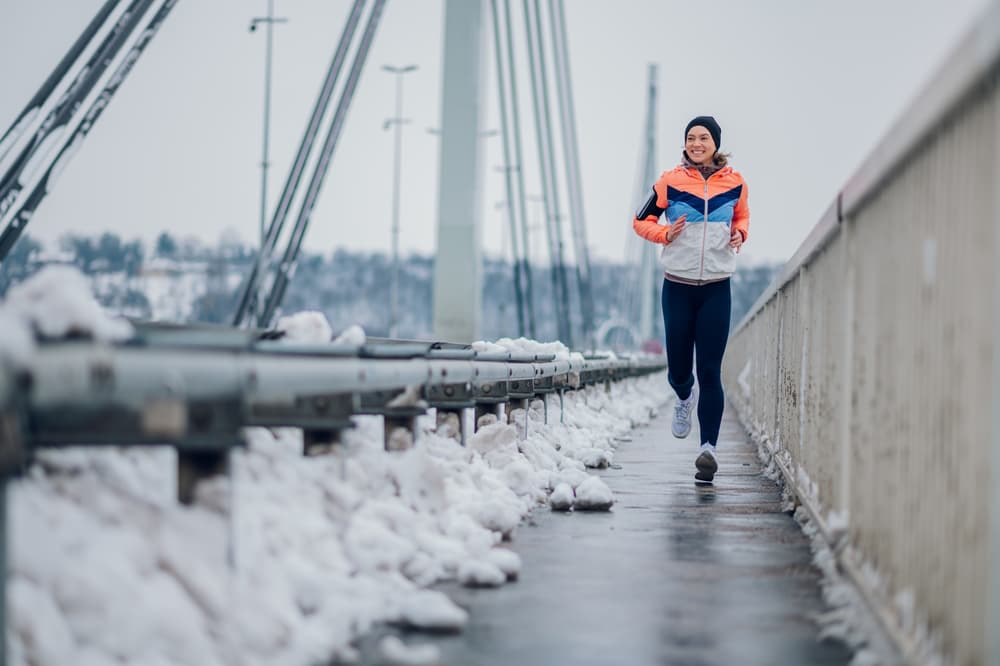
✅ Αθλητές ή άτομα που γυμνάζονται
Ο έλεγχος του βάρους σε αθλητές βοηθά στη βελτιστοποίηση της απόδοσης και στην αποφυγή τραυματισμών, ιδιαίτερα σε αθλήματα που απαιτούν συχνές προσγειώσεις ή στροφές (π.χ. μπάσκετ, τένις, τρέξιμο).
✅ Άτομα μετά από χειρουργείο
Κατά την περίοδο της αποκατάστασης, είναι σημαντικό να μην υπάρξει αύξηση βάρους λόγω ακινησίας, καθώς κάτι τέτοιο επιβαρύνει τις επουλωμένες δομές και καθυστερεί τη λειτουργική αποκατάσταση.

Obesity and orthopaedic issues
Η παχυσαρκία φαίνεται να επιδεινώνει την μυοσκελετική υγεία τόσο εμβιομηχανικά όσο και μεταβολικά. Η παχυσαρκία θεωρείται ότι προκαλεί μια χρόνια, χαμηλού βαθμού, προφλεγμονώδη κατάσταση. Οι υπέρβαροι και παχύσαρκοι ενήλικες έχουν αυξημένους δείκτες φλεγμονής στον ορό. Αυτές περιλαμβάνουν την C-αντιδρώσα πρωτεΐνη, την ιντερλευκίνη-6 και τη λεπτίνη. Αυτές οι κυτοκίνες προέρχονται από λιπώδη ιστό, και είναι γνωστές και ως «αδιποκίνες». Κλινικές μελέτες έχουν δείξει συσχέτιση μεταξύ των επιπέδων της αδιποκίνης και της απώλειας όγκου χόνδρου. Επιπλέον, η λεπτίνη – μια από τις αδιποκίνες – είναι υπεύθυνη για την ενεργοποίηση ενός ενδοαρθρικού προφλεγμονώδους κύκλου που συμβάλλει στη διάσπαση του κολλαγόνου, οδηγώντας έτσι σε επιδείνωση της οστεοαρθρίτιδας.
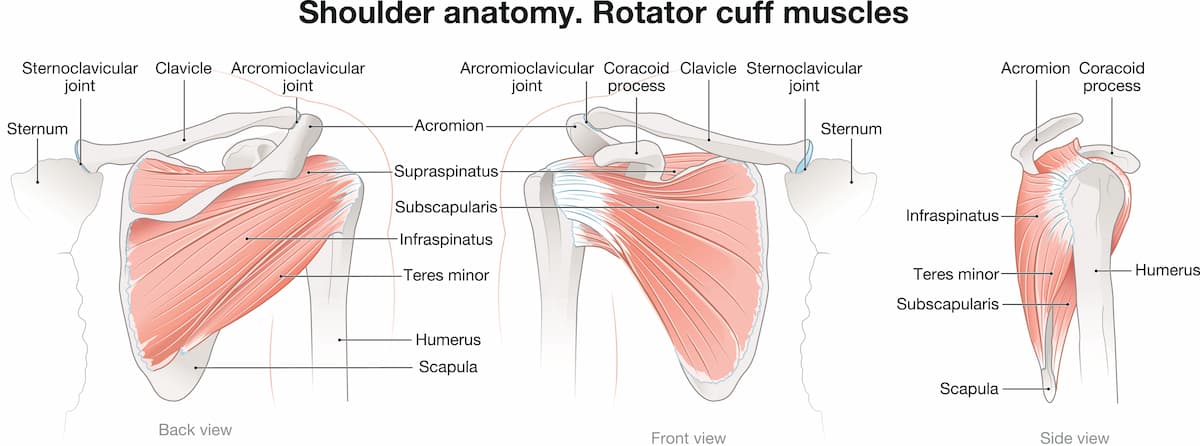
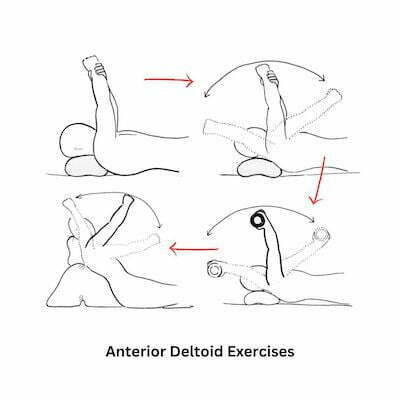
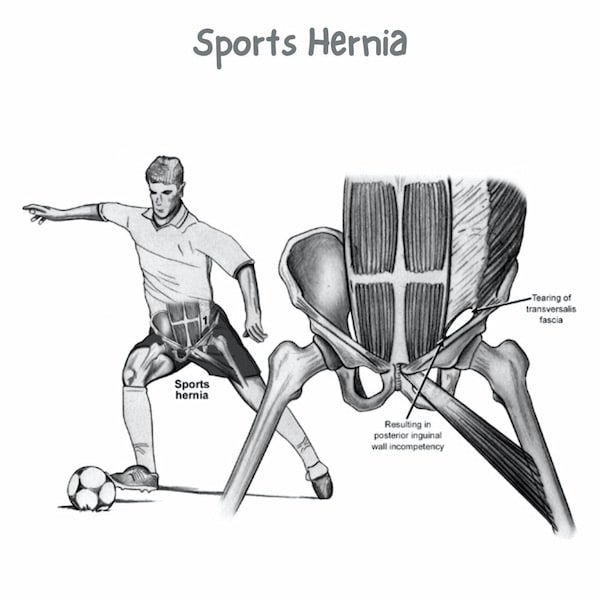
Πολλαπλές μελέτες έχουν δείξει τη συσχέτιση της παχυσαρκίας ως παράγοντα κινδύνου σε πολλαπλούς τραυματισμούς μαλακών ιστών, που πρέπει να λάβει υπόψη ο ορθοπεδικός χειρουργός. Σε ό,τι αφορά στο άνω άκρο, η τενοντίτιδα ώμου και το impingement syndrome ώμου είναι πιο συχνά στον παχύσαρκο πληθυσμό. Επιπλέον, η χειρουργική αντιμετώπιση αυτών των καταστάσεων με αρθροσκόπηση στον παχύσαρκο πληθυσμό έχει δείξει κατώτερα χειρουργικά αποτελέσματα σε σύγκριση με τα μη παχύσαρκα άτομα που υποβάλλονται σε πανομοιότυπες χειρουργικές επεμβάσεις.
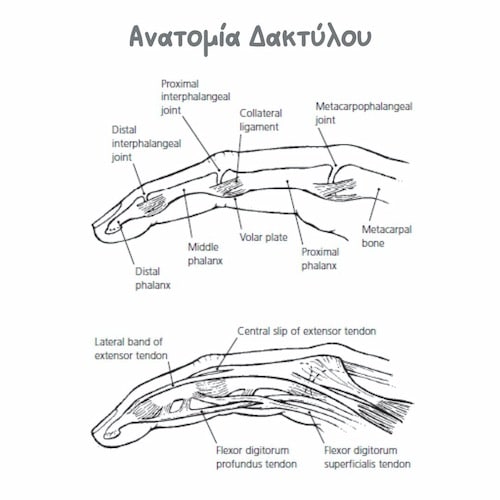
Η συχνότητα εμφάνισης του συνδρόμου καρπιαίου σωλήνα συσχετίζεται με την παχυσαρκία, ωστόσο η απώλεια βάρους δεν βελτιώνει τα συμπτώματα. Αυτό παραπέμπει στον πιθανό αντίκτυπο των μεταβολικών επιδράσεων που αναφέρθηκαν προηγουμένως και στον ρόλο τους στο σύνδρομο καρπιαίου σωλήνα στους παχύσαρκους.
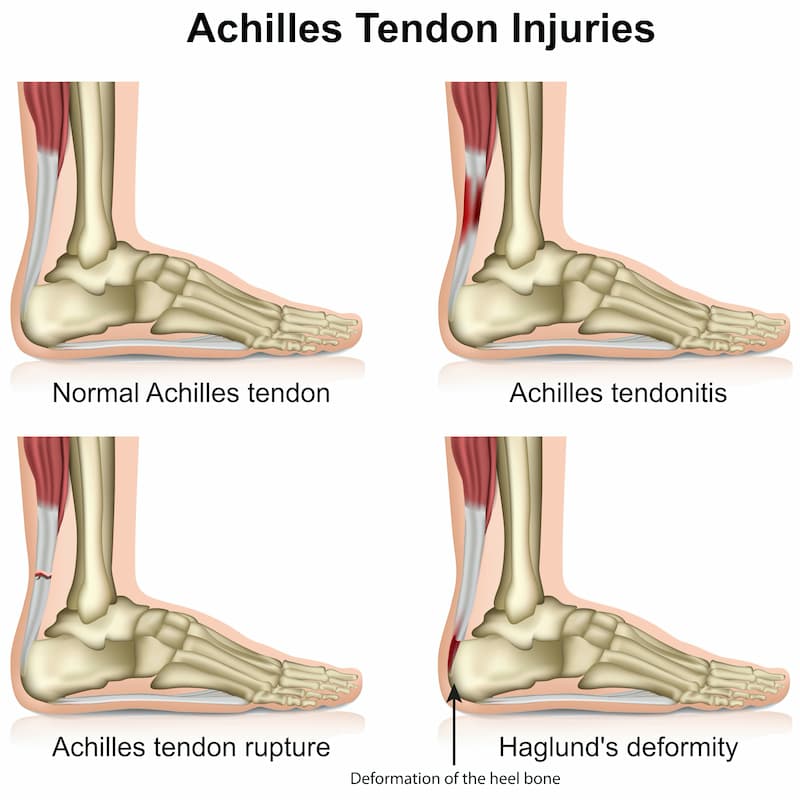
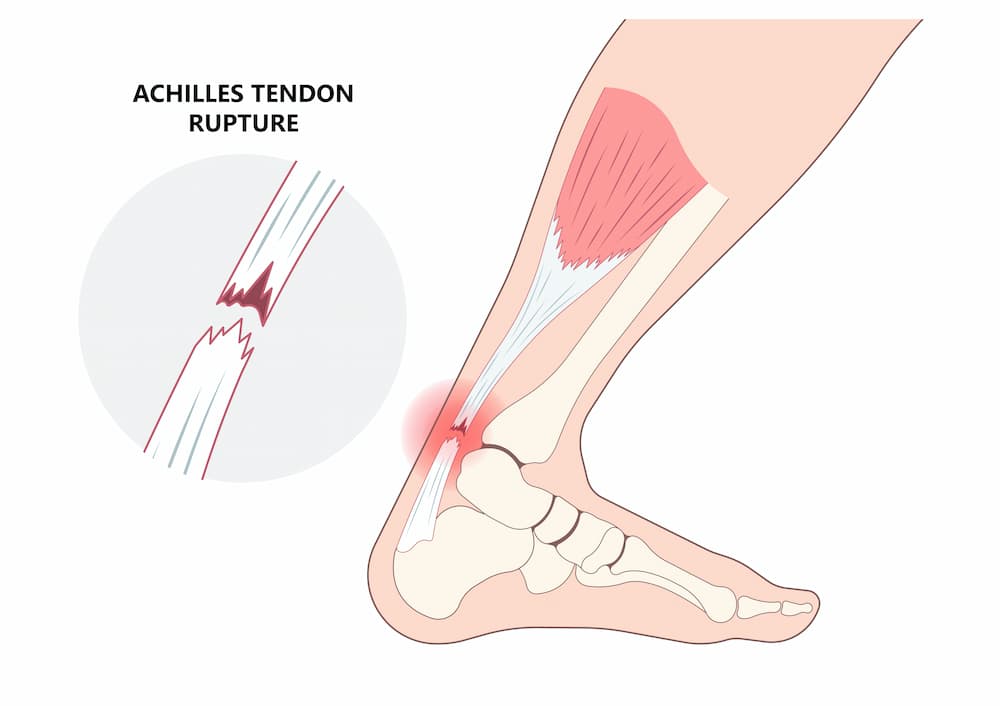
Σε ό,τι αφορά στο κάτω άκρο, η πελματιαία απονευρωσίτιδα, η αχίλλειος τενοντίτιδα και η δυσλειτουργία του οπίσθιου κνημιαίου τένοντα είναι πιο συχνές στον παχύσαρκο πληθυσμό.
Μελέτες έχουν δείξει ότι η παχυσαρκία μπορεί να οδηγήσει σε αυξημένες επιπλοκές στην περιεγχειρητική περίοδο. Η έλλειψη ανατομικών ορόσημων μπορεί να κάνει τη χειρουργική επέμβαση πιο δύσκολη και επιρρεπή σε δυσμενή έκβαση. Η παχυσαρκία αυξάνει επίσης τον κίνδυνο μετεγχειρητικής λοίμωξης, ψευδάρθρωσης, χρόνιου πόνου και αποτυχίας των εμφυτευμάτων. Η μειωμένη αγγείωση στον λιπώδη ιστό μπορεί να επηρεάσει αρνητικά την επούλωση των πληγών. Επιπλέον, συννοσηρότητες που σχετίζονται με την παχυσαρκία, όπως ο σακχαρώδης διαβήτης τύπου ΙΙ, η υπέρταση, η δυσλιπιδαιμία, οι καρδιαγγειακές παθήσεις, το εγκεφαλικό επεισόδιο, η υπνική άπνοια, η ουρική αρθρίτιδα και άλλα, μπορούν να επηρεάσουν αρνητικά την περιεγχειρητική περίοδο, τον κίνδυνο αναισθησίας και το χειρουργικό αποτέλεσμα.
An important step towards better MSK health
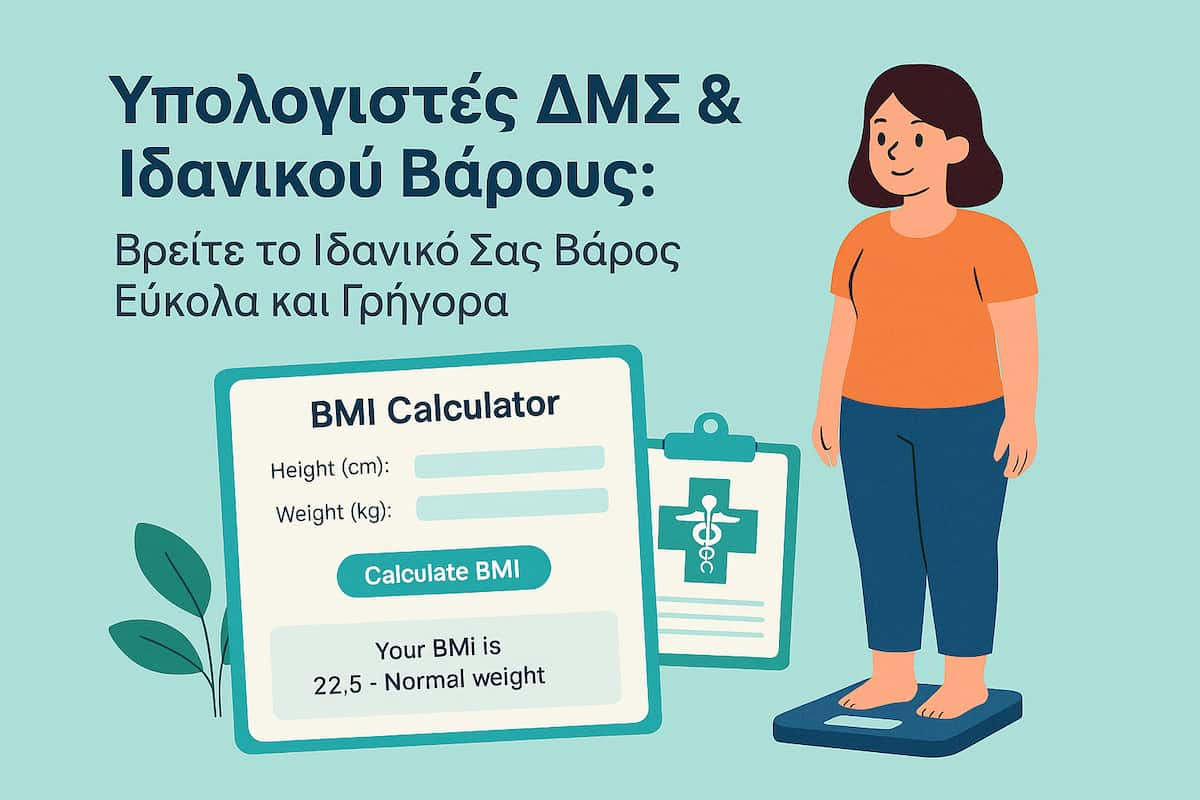
Η χρήση των online υπολογιστών ΔΜΣ και Ιδανικού Βάρους προσφέρει μια εύκολη και άμεση εικόνα της φυσικής σας κατάστασης. Αν και δεν αντικαθιστούν την αξιολόγηση από ιατρό, μπορούν να λειτουργήσουν ως έναυσμα για υγιεινές αλλαγές και να καθοδηγήσουν πιο συνειδητές αποφάσεις σχετικά με τη διατροφή, την άσκηση και τη γενικότερη φροντίδα του σώματος.
🩺 Στην ορθοπαιδική, η πρόληψη ξεκινά από την καθημερινότητα. Μια μικρή αλλαγή στο βάρος μπορεί να φέρει μεγάλη διαφορά στη ζωή των αρθρώσεων σας.

BMI calculator
BMI Calculator
- Κάτω από 18,5: Ελλιποβαρής
- 18,5 – 24,9: Φυσιολογικό βάρος
- 25 – 29,9: Υπέρβαρος
- 30 και άνω: Παχυσαρκία
Ideal weight calculator
Ideal Weight Calculator
FAQs - Frequently Asked Questions
What's BMI?
Το BMI ή Δείκτης μάζας σώματος αποτελεί μία ένδειξη της σχέσης βάρους και ύψους και της εκτίμησης του βαθμού παχυσαρκίας ενός ατόμου. Υπολογίζεται διαιρώντας το βάρος (σε κιλά) με το τετράγωνο του ύψους (σε μέτρα).
How do you calculate ideal weight?
Το Ιδανικό Βάρος υπολογίζεται με βάση το φύλο και το ύψος του ατόμου, χρησιμοποιώντας τύπους όπως ο τύπος Devine.
What's the ideal weight by age & height?
Η ηλικία παίζει σημαντικό ρόλο. Καθώς μεγαλώνουμε, ο μεταβολισμός μας επιβραδύνεται, γεγονός που μπορεί να οδηγήσει σε αύξηση του σωματικού βάρους. Επιπλέον, η μυϊκή μάζα μειώνεται και το ποσοστό λίπους στο σώμα αυξάνεται.
Find us
Book an appointment with us today
Body mass index (BMI) & ideal weight in Orthopaedics Read More »