Shoulder Instability | When do I need surgery?
Shoulder dislocation occurs when our shoulder comes out of the socket. Here we will examine what are the indications for surgery and what are the available surgical solutions, so that we can return to business as usual as soon as possible.
Table of contents
What is shoulder dislocation?
Shoulder dislocation occurs when the head of the humerus moves out of place, losing normal contact with the glenoid cavity of the shoulder blade.
The most common shoulder dislocation is the anterior shoulder dislocation. Rarer types are the posterior shoulder dislocation and the inferior dislocation (luxatio erecta).
How does shoulder dislocation occur?
Most often, shoulder dislocation is the result of trauma, such as a fall on the shoulder, or a blow to the shoulder during a car accident. Dislocation can also occur during sports activities, especially in the case of sports with intense physical contact (football, basketball, rugby). Occasionally, shoulder dislocation can occur in patients with hypermobility of the joints due to loose connective tissue.
What are the lesions associated with a dislocated shoulder?
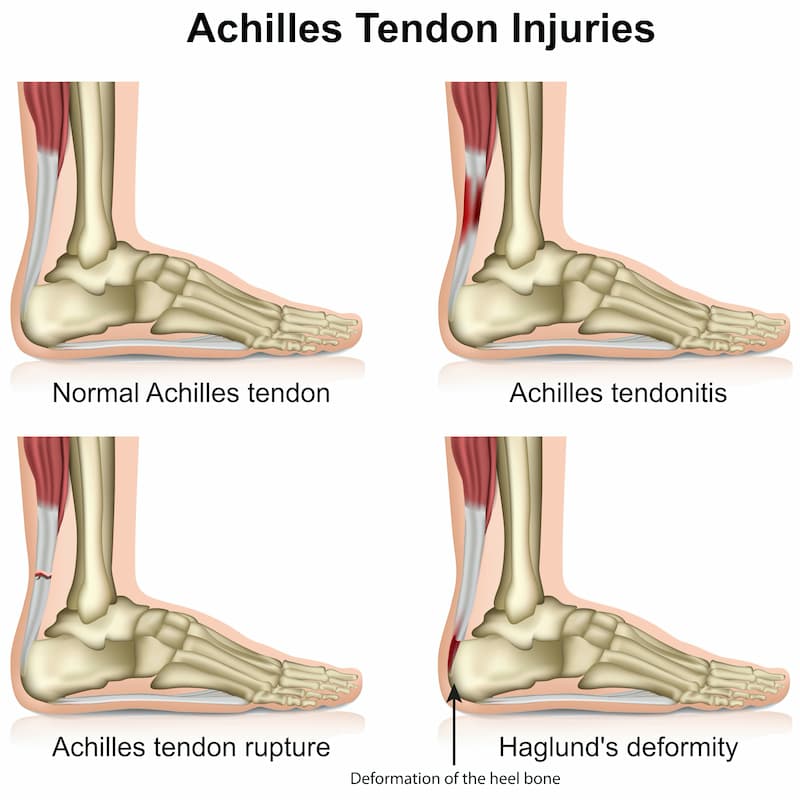
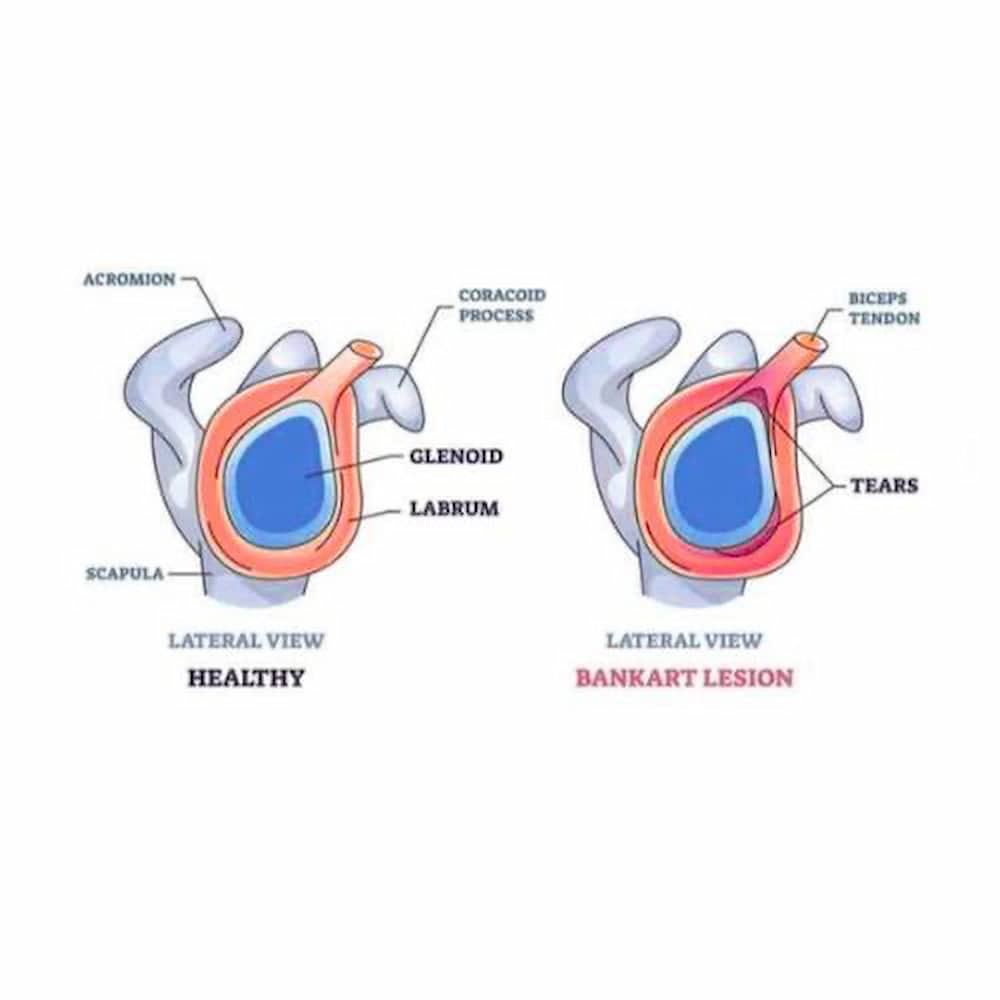
Once a shoulder has dislocated, it is vulnerable to repeat episodes. When the shoulder is loose and slips out of place repeatedly, you develop a condition called recurrent shoulder instability. This is caused by an injury to a structure called the labrum. The labrum is the cartilage rim of the socket of the shoulder blade (glenoid) and represents the bumper of the socket. During the first dislocation, this bumper gets injured and does not heal properly, it scars down and makes the socket shallower. This makes it easier for the shoulder joint to dislocate the next time an injury occurs, or even with trivial injury. This is typically referred to as the Bankart lesion. Another lesion that occurs with shoulder dislocation is the Hill-Sachs lesion. This is an impaction injury or depression of the humeral head, as it catches in the front of the glenoid. This lesion also has therapeutic implication, as it may engage on socket easily, causing recurrent dislocations. In a minority of patients, the shoulder can become unstable without a history of injury or repetitive strain. In such patients, the shoulder may feel loose or dislocate in multiple directions. This is called multidirectional instability. These patients have naturally loose ligaments throughout the body.
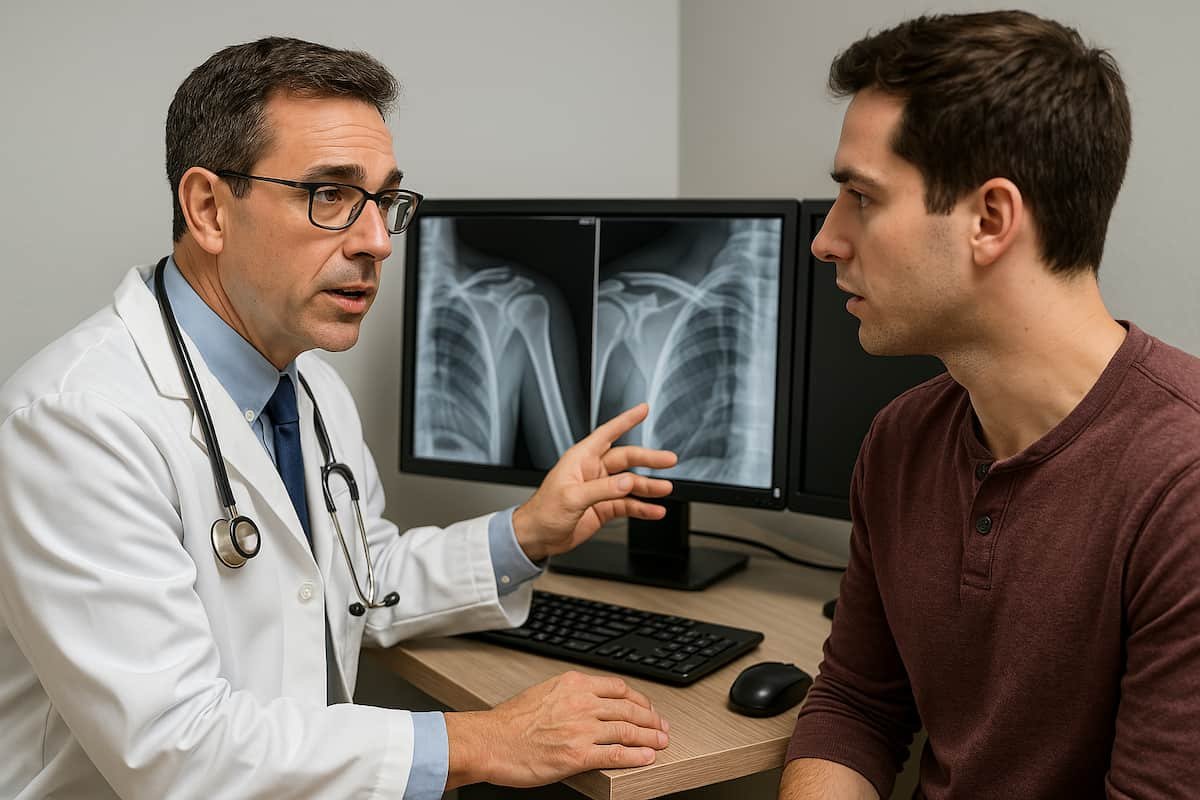
What does diagnosis entail?
The diagnosis of a dislocated shoulder is usually obvious on plain x-rays. In cases of recurrent instability, an MRI scan or MRI arthrogram may be ordered to assess the extent of the soft tissue damage. If there is suspicion of bone loss in the socket, or there are associated fractures in conjunction with the dislocation, a CT scan may be useful as well. In patients over 40-45 years, an ultrasound might be useful, to rule out rotator cuff tears.
What should I do if I dislocate my shoulder?
If you suspect a shoulder dislocation, you shoulder seek immediate medical attention at the closest emergency department. The doctor will examine you, confirm the diagnosis with x-rays, and set your shoulder back into the joint by pulling it with a process called closed reduction. This is usually done under gentle conscious sedation. In some patients, closed reduction under sedation might not work, especially if their muscles go into spasm. In these patients, closed reduction under general anaesthetic may be necessary. Once the shoulder is back in place, any severe pain stops almost immediately. The doctor will order another X-ray to make sure the reduction was successful. Either way, after your shoulder is popped back into the joint, your arm will be placed into a sling for a few weeks. You will then get physical therapy for strengthening. This rehabilitation helps prevent future shoulder dislocations.
After the initial reduction of the dislocation, a specialized evaluation of the patient by a shoulder surgeon is required in order to determine the appropriate treatment.
When do I need surgery?
You may need surgery if:
- You previously had a shoulder dislocation and you are at risk to have it again, because of age (<25 years old) or activity level (contact sports).
- You had a recurrent shoulder dislocation (>2 times)
- You have associated soft tissue injury, such as a rotator cuff tear (common in >40 years old).
- You have associated fractures, such as a glenoid fracture or a humeral head fracture.
If nonsurgical treatments and physical therapy have not helped, surgery is often the next option, to reduce the risk of recurrence and quickly return to your daily activities.
How does surgery take place?
Your age, activity level, and the extent of your injury will help your shoulder surgeon determine which type of surgery is best for you. Most shoulder instability surgeries are performed arthroscopically. An arthroscope is a tiny camera that is inserted through small incisions into the shoulder joint. Shoulder arthroscopy is a minimally invasive procedure that results in minimal pain. Open stabilization surgery, which requires a larger incision, may be necessary if you have a complex problem or are at high risk of recurrent instability.
What are the different types of surgery?
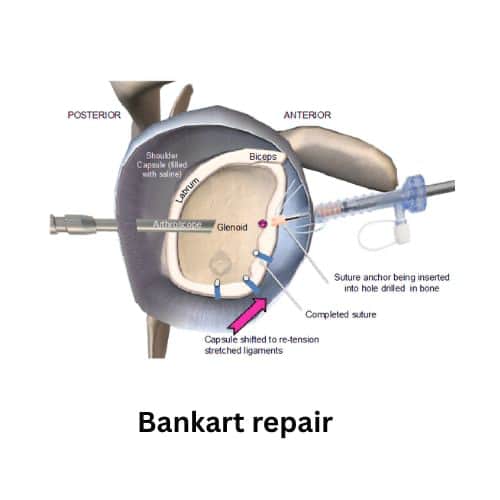
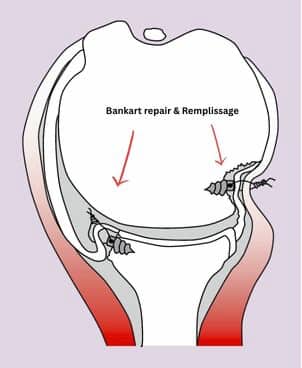
Bankart repair
Bankart lesion is a tear in the labral cartilage of the glenoid fossa, which can be caused by a shoulder dislocation. The tear usually involves the anterior and inferior labral cartilage. The Bankart procedure, usually arthroscopic, repairs the tear and stabilizes the joint, with the aim of preventing recurrence of the dislocation. The arthroscopic technique allows the repair of the damage through small incisions. The repair is done with small suture anchors. At the same time, capsular shift of the anterior shoulder capsule is usually performed to improve joint stability and reduce the risk of recurrence of the dislocation. The arthroscopic technique allows for smaller incisions, minimal blood loss, reduced postoperative pain, and rapid recovery.
Remplissage technique
The Remplissage technique is an arthroscopic procedure used to treat shoulder instability, especially in cases where there is a large Hill-Sachs lesion. It involves placing the posterior capsule (capsulodesis) and the infraspinatus (tenodesis) in the area of the lesion, essentially filling the humeral head defect. This procedure is performed in conjunction with the Bankart procedure.
Latarjet procedure
The Latarjet procedure is a surgical procedure to treat shoulder instability. It involves transferring a bone fragment from the coracoid process (a bone near the shoulder blade) to the glenoid fossa (the part of the shoulder blade that forms the shoulder joint), to enhance the stability of the joint. The coracoid process is fixed to the glenoid fossa with screws or metal buttons. The procedure can be performed open or arthroscopically, depending on the case or the surgeon's preference.

Instead of the coracoid process, other grafts can be used, such as autograft from the pelvis, allograft from the tibia, the distal part of the clavicle, etc.

FAQs - Frequently asked questions
Can this be an outpatient surgery?
Yes, shoulder instability surgery can be done on an outpatient basis, and you can potentially go home the same day.
What's the duration of the procedure?
The procedure may last 1-2 hours, based on the complexity of your case.
Is this surgery painful?
Before surgery, the anesthesiologist will use ultrasound to inject anesthetic medication around your nerves to provide a peripheral nerve block. The medication numbs the area from your neck down to your arm. The doctor may also give you medication to help you sleep during the surgery.
How much will the pain last for after surgery?
A regional nerve block can be short- or long-acting and lasts 18 to 72 hours. Your doctor will also recommend prescription medications, which will minimize your pain as the nerve block wears off. An ice pack will also help with pain at night. Following your doctor’s instructions for pain management will help minimize the need for narcotic painkillers. Most people do not need painkillers after the first few days.
What's the recovery time after this procedure?
How long your recovery and rehabilitation will take will depend on several factors, including the severity of your injury, how long or how often you had shoulder instability before surgery, and how well you keep up with physical therapy appointments and exercises.
How soon will I have to start physiotherapy?
You will likely begin physical therapy within 3-4 weeks after shoulder instability surgery. During the first four to six weeks, range-of-motion restrictions may be used to protect your repair. In the following weeks, you will gradually progress from assisted movement (your physical therapist or your good hand will move your affected shoulder) to light resistance exercises and strengthening exercises.
When can I start driving?
You can usually start driving at six weeks.
Will I have any other activity limitations?
You should limit weight lifting until 12 weeks. You should not participate in contact sports for a few months after surgery.
How soon may I return to sports?
If you are an athlete, your return to play will depend on your specific sport and your progress. Your return should be progressive and meet specific criteria that will be established between your doctor and physical therapists.
Find us
Book an appointment with us today
Shoulder Instability | When do I need surgery? Read More »