Reverse shoulder arthroplasty is a very successful operation that has become extremely popular worldwide in recent years, with very encouraging results. In reverse arthroplasty, the replacement of worn surfaces is reversed relative to normal shoulder anatomy and anatomical arthroplasty. The indications for this operation have expanded dramatically in recent years, with the result that the inversion provides a solution to many complex problems.
Table of contents
What is reverse shoulder arthroplasty | Rationale
Reverse shoulder arthroplasty was developed in the 80s as a solution for rotator cuff arthropathy in older patients. Today, due to its excellent results, it has established itself as the treatment of choice not only for arthritis and rotator cuff arthropathy, but for a number of problems around the shoulder.
The National Registries report a 10-year survival rate of reverse arthroplasty for rotator cuff arthropathy of 94%. The increasing surgical experience with the reverse prosthesis and the subsequent reduction in complications has led in recent years to a spectacular expansion of the relevant indications. According to the Australian Joint Registry, the percentage of shoulder arthroplasties that are reverse has skyrocketed from 42.2% in 2009, to approximately 77.9% in 2018.
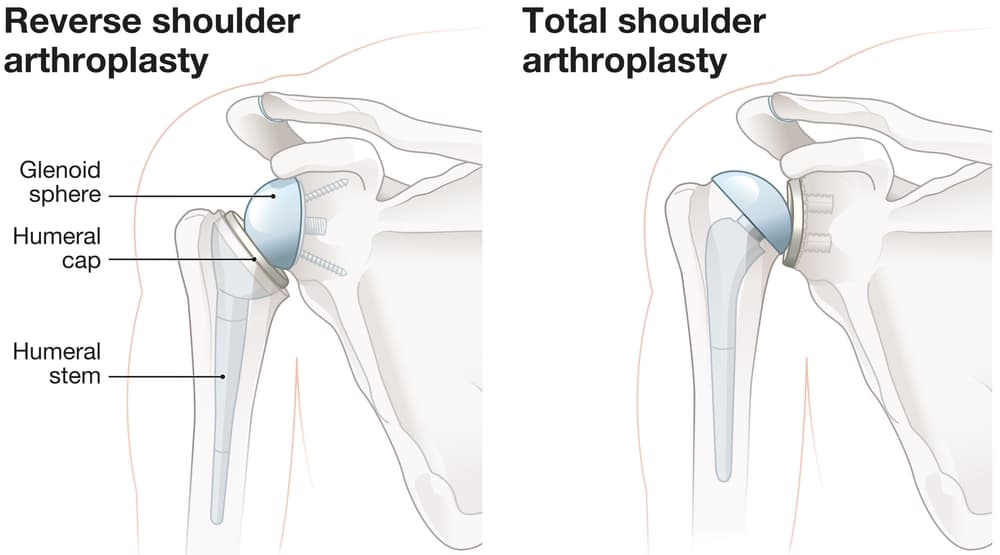
There are 2 main types of shoulder arthroplasty. Anatomic Shoulder Arthroplasty involves replacing the head of the humerus with a metal prosthesis and replacing the shoulder blade with a plastic prosthesis. Anatomic arthroplasty is performed in younger patients with an intact rotator cuff.

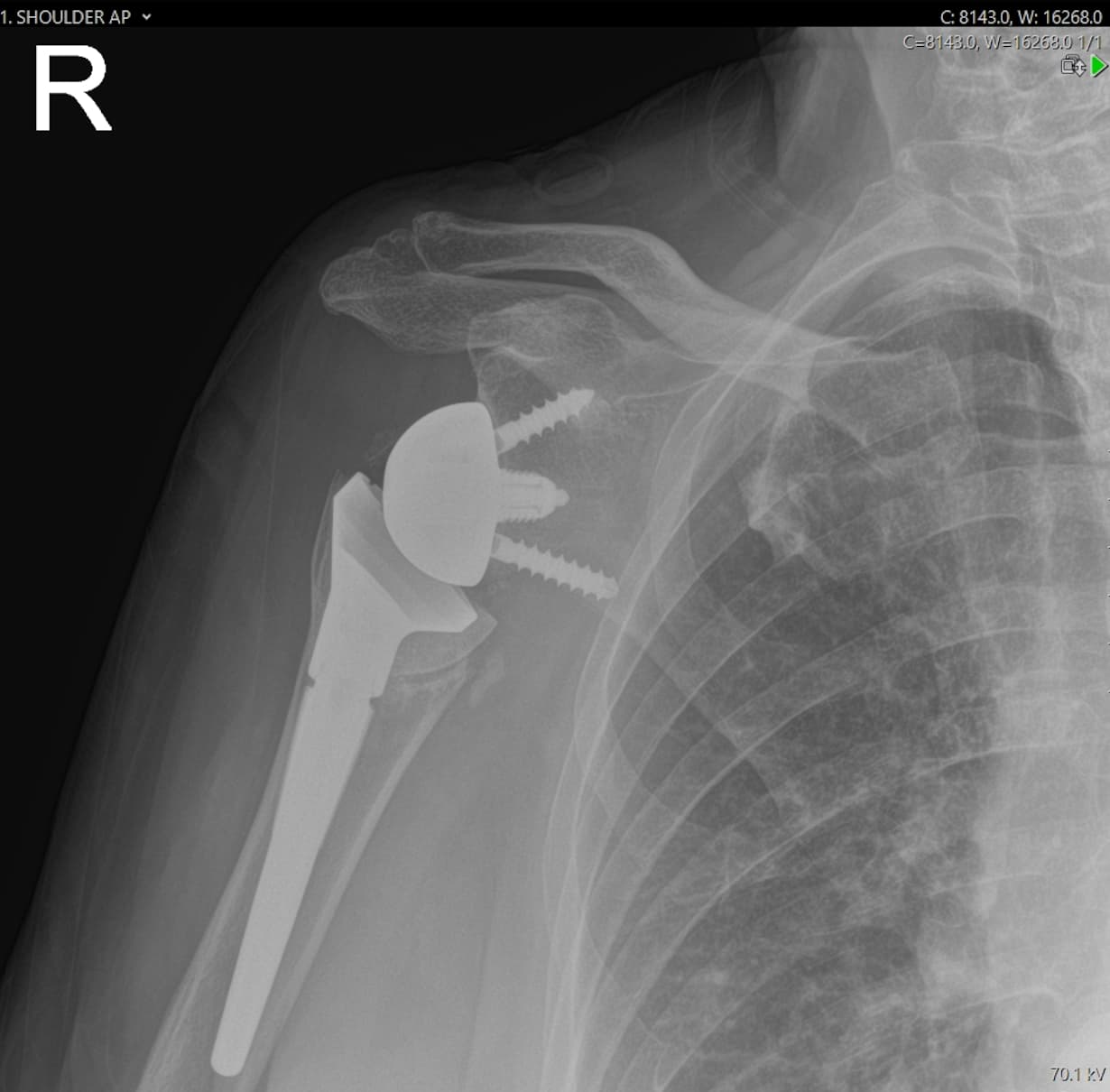
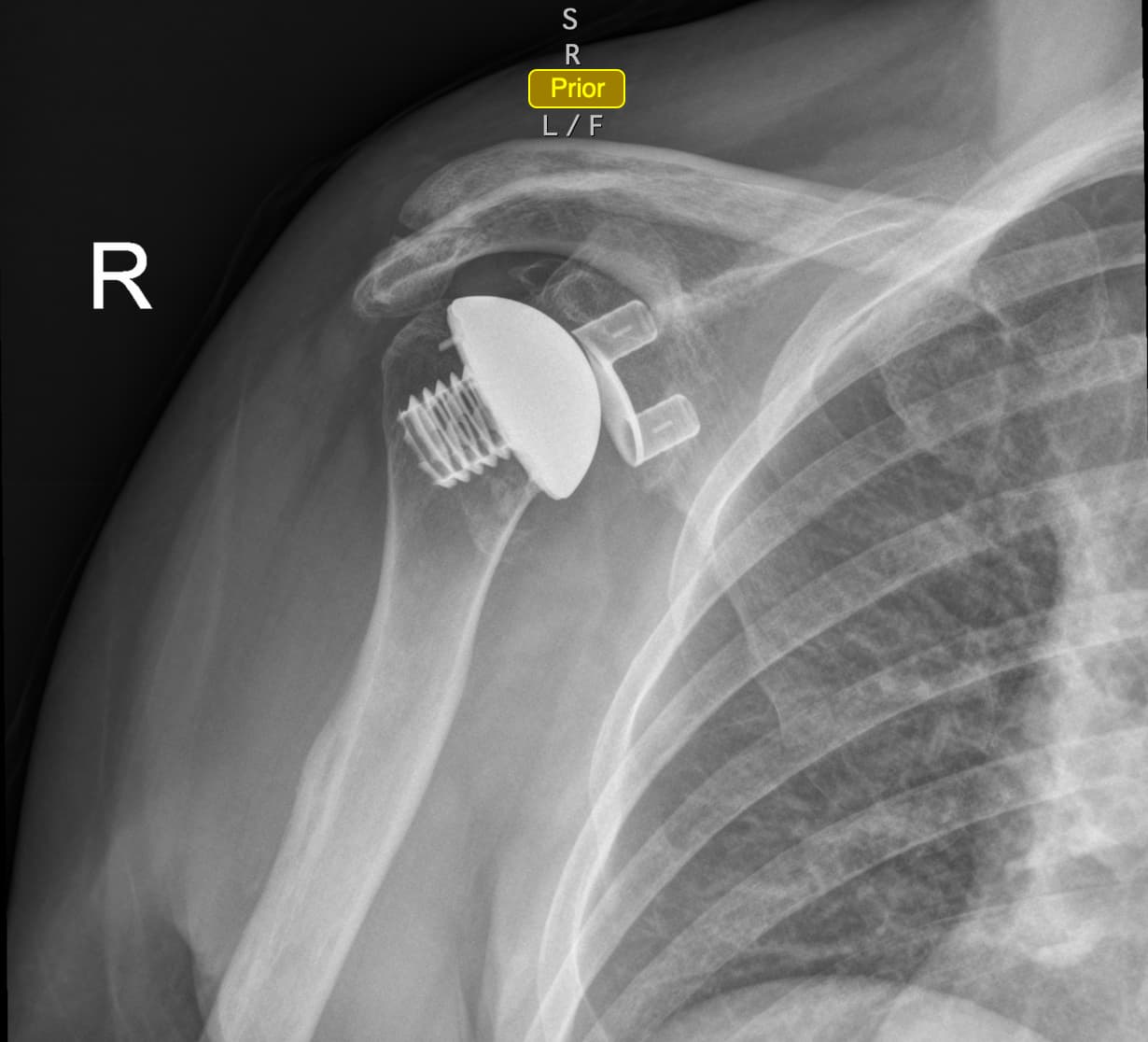
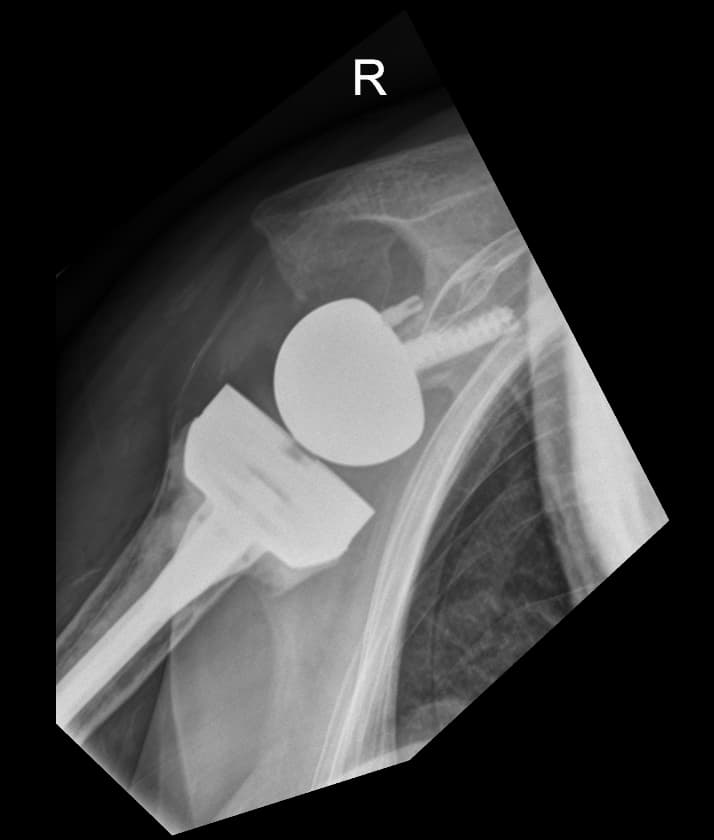
Reverse Shoulder Arthroplasty is performed in patients with arthritis, rotator cuff arthropathy, significant rotator cuff tears, humeral head fractures that are not amenable to internal fixation. In reverse shoulder arthroplasty, the head and concave surface ("cup") are positioned in reverse of normal (glenosphere on the glenoid and concave surface on the humerus).
Other types of shoulder arthroplasty include resurfacing, as well as shoulder hemiarthroplasty.
In reverse arthroplasty, the replacement of worn surfaces is reversed relative to the normal anatomy of the shoulder. While anatomic arthroplasty replicates the normal anatomy, reverse arthroplasty follows a non-anatomic philosophy, with reverse replacement of worn articular surfaces.


The head of the humerus is replaced with a curved prosthesis (cup), while the humerus is replaced with a spherical prosthesis (glenosphere). In this way, the "lever arm" of the shoulder joint is restored, and the patient is able to raise his arm using only the deltoid, without needing the support of the rotator cuff.
Reverse shoulder arthroplasty | Indications
Given the explosion in popularity of reverse arthroplasty, it is not surprising that the indications for placement of this prosthesis have expanded dramatically in recent years. These indications include:
- Osteoarthritis
- Cuff arthropathy
- Massive irreparable rotator cuff tears
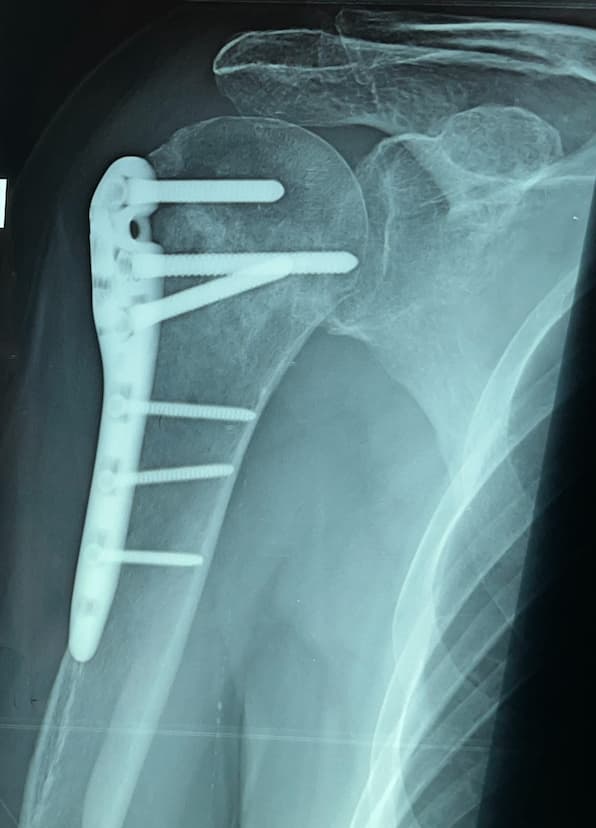
- Trauma – proximal humeral fractures, either acutely, or secondarily.
- Proximal humerus fracture malunion
- Proximal humerus fracture nonunion
- Rheumatoid arthritis
- Avascular necrosis (AVN)
- Post-traumatic arthritis
- Failed rotator cuff repair
- Failed ORIF


Ανάστροφη Αρθροπλαστική Ώμου | Φυσικοθεραπεία
Η αποκατάσταση μετά από ανάστροφη ολική αρθροπλαστική ώμου περιλαμβάνει φυσικοθεραπεία, όπως μετά από κάθε χειρουργείο. Συνήθως ο ασθενής θα φύγει από το νοσοκομείο για το σπίτι με μία ανάρτηση, αλλά κατά κανόνα μπορεί να κάνει σχετικά άμεσα εκκρεμοειδείς κινήσεις και ασκήσεις ανύψωσης στα όρια του πόνου. Η κινητοποίηση είναι σαφώς πιο γρήγορη από την αρθροσκοπικά συρραφή του τροφικού πετάλου, ή την αρθροσκοπικά σταθεροποίηση, καθώς δεν απαιτείται η επούλωση κάποιου τένοντα στο οστό.
Η γρηγορότερη αποκατάσταση αποτελεί μεγάλο πλεονέκτημα, ειδικά σε ασθενείς μεγαλύτερους σε ηλικία, που θα ταλαιπωρούνταν από μια παρατεταμένη ανάρρωση.
Revision shoulder arthroplasty | Causes
A shoulder operation has failed when the results do not meet the expectations of the patient and the surgeon. Failure can result from a number of causes, including stiffness, weakness, instability, pain, or failure to heal, as well as complications, such as periprosthetic infection or nerve injury. Every surgery comes with a risk of failure or post-operative complications, whether it is for a shoulder dislocation, rotator cuff tear, arthritis or fracture.
When a shoulder surgery fails or presents with problems, the patient should consult with a experienced surgeon in the evaluation and management of these conditions. Although pain may seem to be the main problem, it is important to determine the possible mechanical causes of the patient issues, since a mechanical cause can be repaired and reversed.
Before making the final decision to surgically revise a shoulder arthroplasty, it is important to determine the nature of the patient's problems. Common causes of shoulder arthroplasty failure include:
- Periprothetic infection
- Periprothetic fractures
- Adverse reaction to polyethylene or cement (PMMA, polymethylmethacrylate)
- Stiffness
- Bad rehabilitation
- Extra bone - osteophytes not removed, inadequate soft tissue release
- Tuberosity malunion
- Joint overstuffing
- Instability
- Anterior instability
- subscapularis deficiency
- too much glenoid anteversion
- tuberosity malunion
- supra/infraspinatus deficiency
- problem in humeral anteversion or offset
- glenoid bone defect
- Posterior instability
- glenoid retroversion
- posterior cuff deficiency
- problem in humeral retroversion or offset
- glenoid bone defect
- Superior instability
- cuff deficiency
- coracoacromial arch
- Anterior instability
- Nerve injury
- Humeral implact
- malposition
- loosening
- Glenoid
- bone erosion (hemiarthroplasty)
- malposition
- loosening
Reverse arthroplasty provides a solution to the most common problems that an anatomical arthroplasty or a hemiarthroplasty can bring about over time, such as the gradual erosion of the glenoid (glenoid wear), or the secondary rotator cuff deficiency, which are also the most frequent reasons for revision. Also, rTSA is the treatment of choice in cases of failure of previous surgery, such as arthroscopy for tendon suturing, or failure of fixation of a humeral head fracture.
Shoulder arthroplasty infection is a difficult case, often requiring a 1- or 2-stage revision. The first stage usually involves removal of the previous prostheses and placement of a cement spacer, often impregnated with appropriate antibiotics. This is followed by targeted antibiotic therapy for 6 weeks, based on samples sent to the laboratory for culture. Finally, the second stage involves placing a new prosthesis.
Revision Shoulder Arthroplasty is a very demanding surgery and requires an Orthopedic Surgeon with extensive experience in similar cases. It also requires appropriate preparation and study, with careful preoperative planning, imaging, laboratory testing, and many times the participation of a wider therapeutic team, which may, in addition to the shoulder surgeon, include a musculoskeletal and interventional radiologist, an infectious disease specialist, a pathologist, and other specialties, depending on the needs of the patient (MDT, or multidisciplinary team).
Dr Panagopoulos has extensive experience in revision shoulder arthroplasty, having served as an active member in a revision surgical center abroad. This operation must only be performed by a specialized Orthopedic Surgeon with relevant experience, with an organized surgical and medical team, in a specialized hospital with the necessary logistical infrastructure and workforce. Contact us today to learn more about revision and reverse arthroplasty.
FAQs - Frequently Asked Questions
What are the indications for reverse shoulder arthroplasty?
– Shoulder arthritis
– Massive rotator cuff tears
– Proximal humerus fractures
– Avascular necrosis (AVN)
– Malunion/nonunion
– Failed RCR or ORIF
When do I need revision shoulder arthroplasty?
– Periprothetic infection
– Periprothetic fracture
– Prior failed arthroplasty
Find us
Book an appointment with us today

