Pain in the back of the ankle or foot is often the result of problems along the course of the Achilles tendon, or where it attaches to the heel. Achilles tendon disorders range from chronic overuse conditions that lead to inflammation and degeneration of the tendon (Achilles tendinitis), to acute injuries from sports or other activities (Achilles tendon rupture).
Table of contents
What's the achilles tendon?
The Achilles tendon is located at the back of the ankle and connects the calf muscles to the heel bone. Facilitates activities such as walking, running and jumping. The Achilles is the largest and strongest tendon in our body. Subject to 2-3 times body weight during normal walking and 3-6 times body weight or more with running and jumping activities.


Achilles tendinopathy
Achilles tendinitis is a chronic condition characterized by pain and often swelling in the Achilles tendon. The symptoms are due to swelling and inflammation of the tissue surrounding the Achilles tendon.
What are the types of achilles tendonitis?
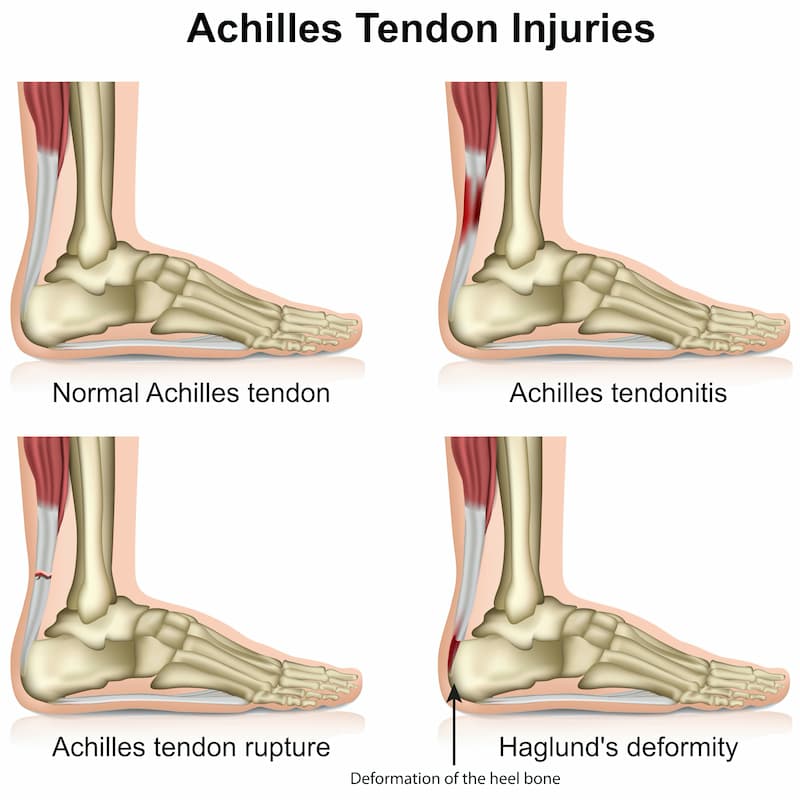
There are 2 main categories of tendinopathy and Achilles tendinitis:
- Non-insertional Achilles tendonitis : In classic Achilles tendonitis, symptoms of pain and swelling are typically located 2-6 cm above the insertion of the Achilles tendon on the heel bone.
- Insertional achilles tendonitis: In this type, the pathology is located in the adhesion of the Achilles tendon to the heel bone. A bony prominence of the heel, or Haglund deformity, is typically found in these cases.

Achilles tendonitis - Symptoms
Symptoms of Achilles tendinitis can vary depending on the severity of the condition.
Typical symptoms include:
- Pain and stiffness in the Achilles tendon, especially in the morning, or after periods of inactivity.
- Pain that worsens with activity, or exercise
- Swelling and tenderness in the tendon
- Creaking sensation during movement in the ankle
- Swelling or thickening in the Achilles tendon near the heel
- Haglund deformity
Diagnosis - Clinical exam
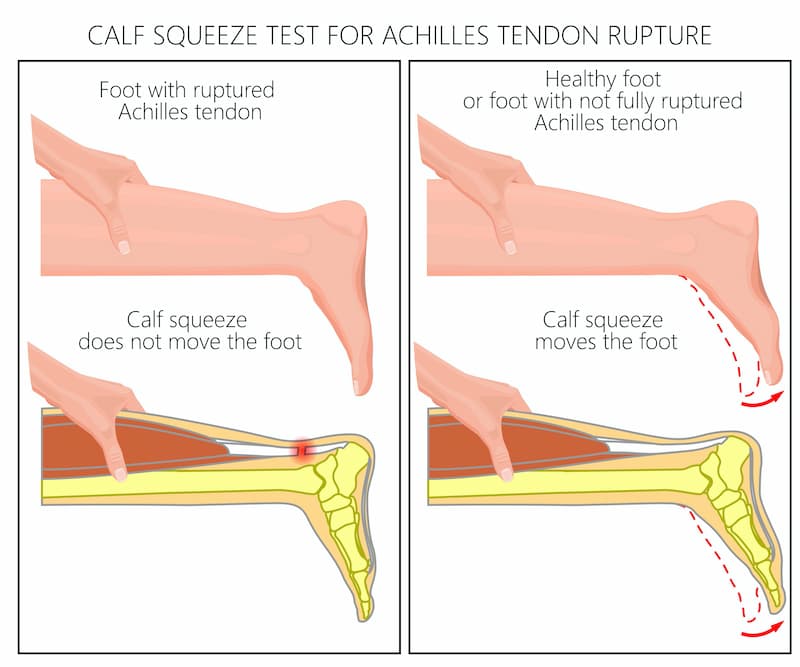
Examination will usually reveal swelling and tenderness around the Achilles tendon. The doctor may detect swollen, inflamed tissue. If there has been any type of associated injury, it is important to ensure that the tendon is intact and that the problem is not, in fact, a ruptured Achilles tendon. This is done by performing the Thompson Test, where the patient lies face down with their legs hanging over the edge of the bed. The calf muscle is then compressed and the foot must move into plantar flexion if the Achilles is intact.

Diagnosis - Imaging
X-rays will usually be negative in non-enveloping, classic Achilles tendinitis, unless there is calcification of the Achilles tendon, which is relatively rare (more common in older patients). However, for catatrophic Achilles tendonitis, a heel osteophyte may be seen on radiographs. An MRI can provide a detailed picture of the soft tissues, but is usually not indicated for the initial evaluation of Achilles tendonitis unless the doctor is trying to answer a specific question (maybe the tendon has ruptured tendon;). If needed, ultrasoundcan also be used, as it is more readily available and less expensive than an MRI.
Achilles tendonitis - Conservative treatment
Most patients with Achilles tendinitis can be effectively treated with non-surgical treatment. This usually involves a period of rest for symptoms to subside, followed by a gradual return to normal activities. Elements of conservative treatment may include:
- Activity Modification. In the short term, they may need to stop any activities that may be making the problem worse. This includes running, jumping, walking up hills, climbing stairs repeatedly.
- Shoe modification. It is important to avoid shoes that aggravate the symptoms. In general, wearing well-fitting and comfortable shoes is beneficial. A few shoe modifications may also be helpful. Some patients feel more comfortable wearing insoles. An increased heel height tends to take some of the load off the Achilles tendon.
- Drugs. Nonsteroidal anti-inflammatory drugs (NSAIDs), 1-3 times a day, can help relieve symptoms in the short term and break the cycle of pain and discomfort. However, for successful long-term management, NSAIDs usually need to be combined with other treatment strategies.
- Stretching of the gastrocnemius and Achilles. A tight muscle increases the force passing through the Achilles tendon and predisposes to microtears. A consistent program of calf stretches is an important part of treatment.
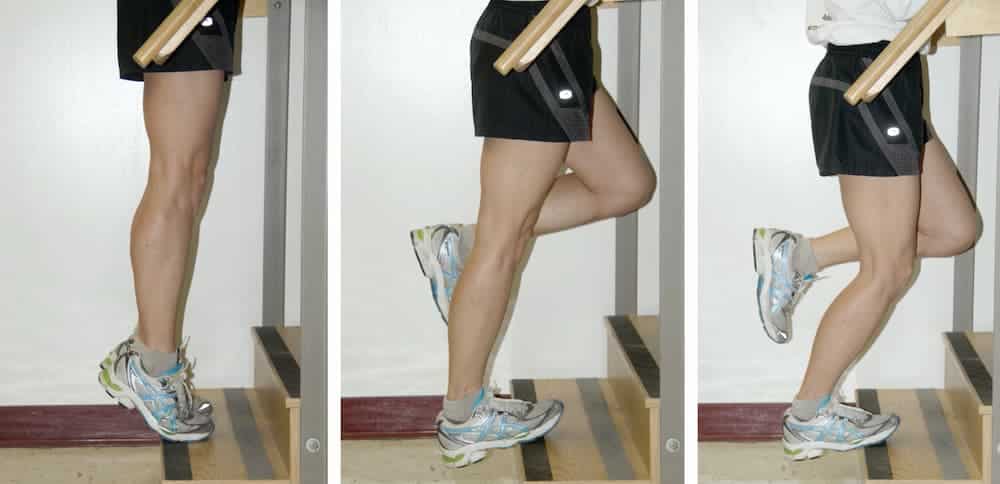
- Double leg heel rises. A high-rep, low-resistance strength program can be very helpful. Perform double heel raises while standing on the edge of the stairs (for more ankle movement). Start with 5 sets of 5 reps, and slowly progress to 10 sets of 15 reps.
- Heel drops. Eccentric Achilles Tendon Exercises: Controlled exercises where the Achilles tendon is lengthened have been shown to be very helpful in improving symptoms. Patients should progress up to performing 5 sets of 10 repetitions. These exercises should be performed 5-6 days a week during the active treatment phase, and 3 times a week thereafter, to minimize the chance of relapse. It is critical that this exercise be done carefully. Patients should always warm up first (eg exercise bike for 5-10 minutes) before performing these exercises to avoid injury.
- PRP Injections. It has been suggested that injecting PRP, taken from the patient's own blood, can stimulate healing. However, there is a lack of evidence to confirm that PRP injections are more effective than traditional treatment options. Cortisone injections are generally not recommended, due to the increased risk of weakening or even tearing the tendon.
Achilles tendonitis - Surgical treatment
Surgical treatment of Achilles tendinitis is rare. Surgery is indicated only when appropriate conservative treatment has failed. Patient compliance and postoperative management are important factors in preventing ankle stiffness or recurrence of symptoms.
Surgery usually requires removal of the damaged tissue and surgical repair of the tendon. In some cases of extensive damage, a local healthy tendon transfer (tendon transfer) is performed to strengthen the diseased Achilles tendon. Postoperative immobilization is required, followed by gradual introduction of range of motion and strengthening exercises. It may take 3-6 months to achieve full recovery. Some known complications are recurrence and ankle stiffness.
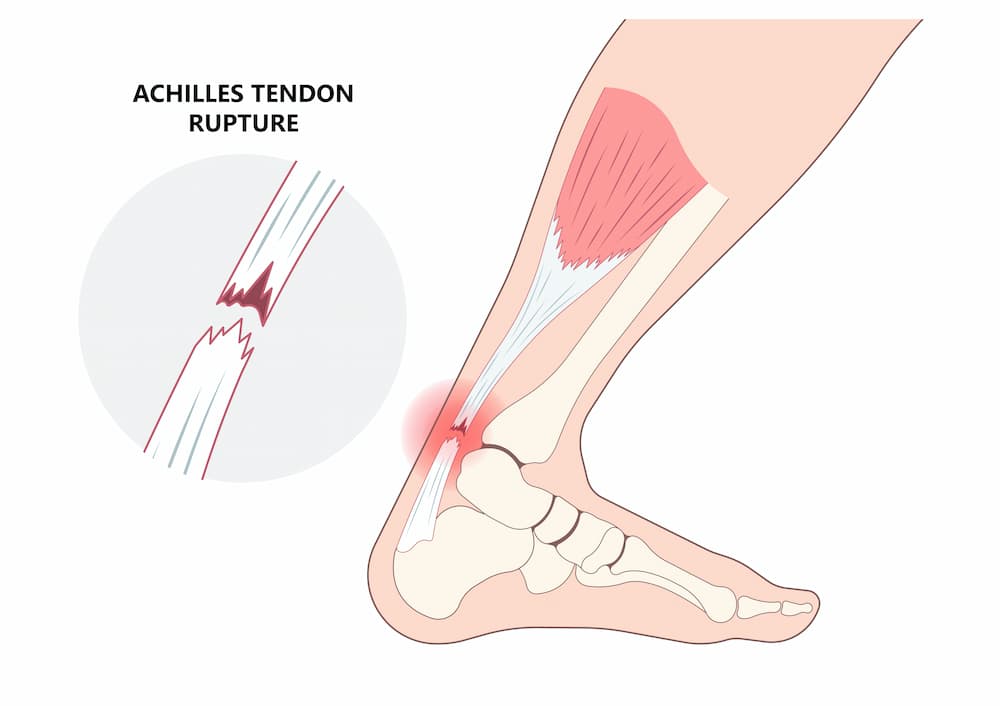
Achilles tendon rupture
Achilles ruptures usually occur in athletic people in their 30s, 40s and 50s. However, there is also a small group of patients in their 70s and 80s who suffer from this injury. The injury usually occurs after a sudden application of force resulting in the rupture (rupture) of the Achilles tendon.
Regaining normal Achilles tendon function is important to resuming an active, healthy lifestyle. Achilles tendon rupture can be successfully treated conservatively or surgically. Recent studies indicate that nonsurgical and surgical treatment of Achilles tendon ruptures produce equivalent results.
Patients who undergo surgical treatment for an Achilles tendon rupture can expect a faster return to a pre-injury activity level and a lower rate of re-rupture. However, surgery carries risks of complications such as infection or wound healing problems. For this reason, conservative treatment may be preferable, especially in patients with diabetes, vascular diseases and long-term smokers.
Mechanism of injury
The Achilles tendon receives the maximum load when the calf muscle contracts while simultaneously moving the ankle upwards (dorsiflexion), which causes the tendon to lengthen (eccentric loading). This can happen when changing direction, starting to run, stopping suddenly, or landing from a jump. This sudden increased force through the tendon can lead to a tear, in the same way that a stretched rubber band can break.
The patient with Achilles rupture feels a intense and acute pain in the back of the leg. Depending on the activity, patients often describe the sensation of being "hit in the back of the leg" with a ball, bat, or kick. Tendon rupture can be extremely painful. The injury may be accompanied by swelling and ecchymosis in the area.
Immediately after the injury, the pain varies. Some describe very little or no pain, while others describe a lesser but persistent discomfort. Sometimes there may be an inability to walk. It is very rare for an Achilles tear to be partial. However, a painful Achilles tendinitis or a partial tear of the gastrocnemius can also cause pain in this area. Examination by an experienced orthopedic surgeon is essential to confirm the correct diagnosis.
Diagnosis
The diagnosis of Achilles tendon rupture is easily made by physical examination. Usually, there is a gap in the Achilles tendon at the site of the tear that can be felt by lightly palpating the area. However, the main test to determine if the Achilles has ruptured is the Thompson test. This essentially involves placing the patient in a prone position and compressing the calf. If the Achilles is intact, the foot will lift (plantar flexion). If it is torn, the leg will not move and will tend to be in a lower position.
Plain radiographs may show a blur or shadow on the lateral view. However, more often plain x-rays are normal as the injury is to the tendon and therefore does not affect the bones of the foot. Imaging with ultrasound or MRI confirms the diagnosis.
Achilles tendon rupture - Treatment
Achilles tendon ruptures can be treated both conservatively and surgically. Both treatment approaches have advantages and disadvantages. Recent studies suggest that conservative and surgical treatment of Achilles tendon ruptures produce equivalent results in many. However, the decision on how to treat an Achilles tendon rupture must be based on each patient individually, with an individualized approach. A neglected Achilles tendon rupture can lead to chronic weakness, lameness, and often secondary problems with the knee, ankle, and foot.
Conservative treatment
Conservative treatment of Achilles tendon rupture consists in placing and immobilizing the foot in equinus until the tendon heals. This usually involves some type of boot (cam walker) with a heel lift with insoles or wedges, or a cast.
The primary advantage of conservative treatment is that there are no problems with healing or infection since no surgical incisions are made. Wound infection after Achilles tendon surgery can be a devastating complication, and therefore, for many patients, especially those with diabetes, vascular disease, and long-term smokers, nonsurgical treatment should be considered.
The main disadvantage of non-surgical treatment is that recovery is slower. The overall effect of long-term immobilization and the deviation from "normal" activity for each individual patient must be considered. Surgical treatment may allow faster loading. Additionally, the relapse rate appears to be higher with conservative treatments.
Surgical Treatment
The surgical treatment of Achilles tendon tears involves making an incision in the center of the tendon tear. The tendon is then repaired using sutures in such a way that the ends of the tendon touch. Both open and percutaneous techniques are described. The minimally invasive Achilles rupture repair technique has been shown to be equivalent, but with fewer wound complications and infection than the standard open technique, although with a higher risk of nerve injury. Surgical repair allows faster loading and mobilization. Individualized physical therapy is important to restore strength and balance after surgery.
The advantages of Achilles tendon repair surgery include:
- Quicker recovery
- Early motion
- Lower rerupture rate - recurrence rate is 2-5% with surgery, as opposed to 8-12% with conservative treatment.
The main disadvantage of surgical Achilles tendon tear repair is the potential for surgical complications, such as healing problems, infection, or painful scarring.
FAQs - Frequently Asked Questions
What's the achilles tendon?
The Achilles tendon is located at the back of the ankle and connects the calf muscles to the heel bone. Facilitates activities such as walking, running and jumping. The Achilles is the largest and strongest tendon in our body.
What are the most common achilles problems?
Achilles tendon disorders range from chronic overuse conditions that lead to inflammation and degeneration of the tendon (Achilles tendinitis), to acute injuries from sports or other activities (Achilles tendon rupture).
What are the types of achilles tendonitis?
Insertional & non-insertional achilles tendonitis.
How can we test for achilles tendon rupture?

This is done by performing the Thompson Test, where the patient lies face down with their legs hanging over the edge of the bed. The calf muscle is then compressed and the foot must move into plantar flexion if the Achilles is intact.
What are the advantages of surgery?
Quicker recovery, early motion, lower re-rupture rates.
What are the disadvantages of surgery?
Higher complications rates.
Find us
Book an appointment with us today