If you are an athlete, you know that there are many reasons for playing a sport. The reasons vary from maintaining a healthy body weight, the well-being and endorphin rush that exercise provides, to socializing and enhancing team building and leadership skills.
But in order to be able to participate in sports activities safely, we should also treat our bodies with the necessary respect. Taking proper care of your body and being aware of your limits is key to avoiding mishaps, whether you're a competitive athlete or a weekend warrior.
Our first question after a sports injury is usually: “When can I get back to playing?” The answer to this question varies depending on the type and extent of the injury.
In the following article, we will take a look at the most common sports injuries and their causes.
Table of contents
ACL tears
The ACL or anterior cruciate ligament is one of the most important knee ligaments and is located in the center of the knee. Its main function is to maintain knee stability and prevent the tibia (leg bone) from moving forwards. An ACL tear is one of the most common knee injuries. It also manifests frequently in association with other injuries, such as MCL tears, a torn lateral meniscus, or a PLC (posterolateral corner) injury.
ACL injuries are very common in sports that require a sudden “start-stop” or a sudden change of direction, pivoting or jumping. These sports include football, basketball, skiing, squash, etc. The mechanism of injury typically includes an external twisting motion in a bent and loaded knee. You can have this if you get tackled, stop suddenly from running or land awkwardly after a jump.
When the ACL tears, patients typically feel severe pain accompanied by a snap or pop, and the knee gives way and feels unstable. The knee also becomes very swollen very quickly. Patients are usually unable to weight bear immediately after the injury.
The diagnosis is confirmed by magnetic resonance imaging (MRI), which allows imaging of accompanying soft tissue injuries, such as medial collateral ligament injuries, external meniscal tears, or posterior and external angle tears. It is noted that a meniscal tear combined with a cruciate tear is extremely common.
Initial management typically involves rest, ice, anti-inflammatory medications and physiotherapy. Up to 1/3 of patients will be ok with this treatment, eventually strengthen their muscles and circumvent the ACL-deficient, potentially more unstable knee.
Some patients will do initially well, but will be unable to resume sport activities to the pre-injury level and eventually might need surgery. The decision in that case boils down to their athletic aspirations. Some other patients will have a persistently wabbly knee and will need surgery.
Meniscal tears
Each knee has 2 C-shaped pieces of cartilage between the femur (thigh bone) and the tibia (leg bone), the medial and the lateral meniscus. The medial meniscus is on the inside and the lateral on the outside of the knee. The menisci look like potato wedges. The menisci act as shock absorbers and load sharers. They are the cushions of the knee joint. A torn meniscus is one of the most common knee injuries.
Meniscal tears can usually develop in one of 2 ways, traumatic in the young and degenerative in the old. In younger (<40 years) and active individuals, a torn meniscus can result from forceful twisting of the knee, such as a sudden “stop & turn”, or sudden pivoting of the knee. Essentially what happens is that you twist your bended knee while you put your weight on it. Certain sports increase the risk of this happening, such as tennis, squash, football and skiing. In older people (>40 years), the menisci start to become weaker and more friable and can tear more easily, even without significant trauma. In fact, many of these occur spontaneously or with innocuous activities, such as kneeling or squatting while you do your house errands or your gardening.
Common symptoms include:
- Sharp pain on the inside or outside of the knee, depending on the involved meniscus
- Pain on deep sitting or squatting, if the back part of the meniscus is involved
- Sometimes there can be a dull ache rather than sharp pain
- Painful clicking and catching or locking. If your knee is locking, you might have an unstable torn meniscus that needs more urgent medical attention
- Your knee may also feel like giving way
In case of suspicion of a meniscal tear, the imaging method of choice is magnetic resonance imaging (MRI) of the knee, which also allows the diagnosis of possible accompanying injuries, such as ACL tears.
If you have an isolated torn meniscus and your symptoms are mild, you might opt for conservative management. This will involve rest, avoiding activities that aggravate your knee as well as physical therapy.
In younger patients, bigger tears, or evidence of locking, arthroscopic treatment may be more appropriate.
Ankle sprains
An ankle sprain is an injury that occurs when the ligaments in the ankle joint are stretched or torn. These ligaments hold the bones of the ankle together and help stabilize the joint. Sprains occur when the foot turns excessively in one direction, i.e. moves beyond normal limits. It is the most common cause of ankle pain.


Causes
Causes of sprains include sports injuries – sports with frequent landings from jumping or frequent changes of direction, eg basketball. A sprain can be caused by a simple everyday injury, eg tripping or twisting (my leg turned).
Symptoms & diagnosis
Symptoms of a sprain include swelling, bruising, pain and inability to walk. The diagnostic approach may include an X-ray to rule out the possibility of a fracture. MRI may be needed in chronic cases, in order to rule out ligament insufficiency, osteochondral lesions, or for preoperative planning.
Treatment
Initial treatment includes rest, ice, elevation of the leg, elastic banding, and pain medication, or nonsteroidal anti-inflammatory drugs. In some cases, offloading with crutches, or immobilization for some time may be necessary. In some cases, surgery may be needed to restore ligaments, remove loose bodies or treat cartilage damage.
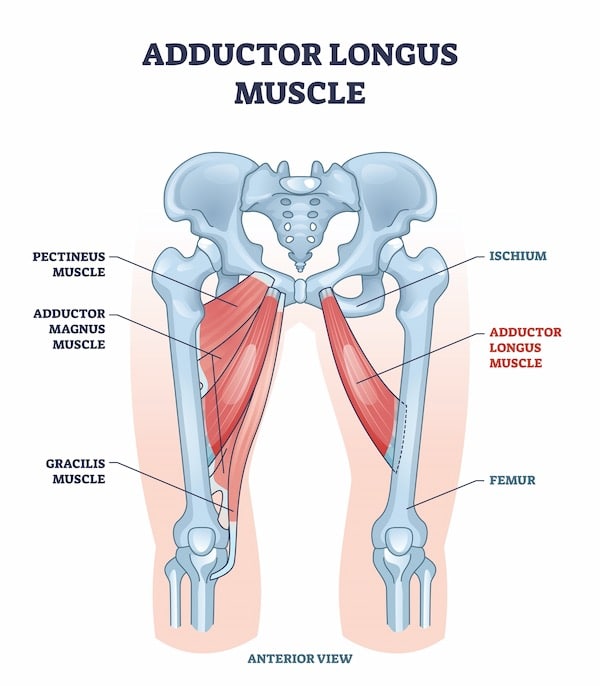
Adductor injuries
Adductor strain is a common injury in athletes. It is characterized by stretching, partial or total rupture of one or more of the adductor muscles (brevis, magnus & adductor longus). The adductor longus is most commonly involved. The adductors stabilize the pelvis and move the legs toward the center of the body (adduction).
The adductors are especially strained during sports activities after repeated changes of direction. If a sudden contraction occurs, particularly great violence may be induced at the point of origin of the muscle, causing rupture of muscle fibers or leading to bone swelling. Passively, rupture can also occur with overstretching. Rupture can be classified in 3 types depending on severity.

Causes
Damage can be caused by a sudden contraction, a sudden change in direction, or a lack of warm-up. Older athletes are more susceptible.
Clinical exam
Athletes usually describe a sharp, piercing pain in the inner thigh during the injury. In mild damage, they can continue the sport, but in type II damage they stop, or start to limp. In type III, the symptomatology is acute (heaviness in the groin, difficulty rising from a chair, or limping when walking).
Treatment
- RICE protocol (Rest, ICE, Compression, Elevation)
- Mild groin stretching exercises, if pain allows
- Kinesiotapping, for offloading
- Exercise program focused on stretching and strengthening
- Gradual return to individual and team training
Sports hernia
Abdominal pain can occur after an injury during sports activity, but it can also be the result of persistent exercise or abdominal strain. This damage is often known as groin pain, sports hernia, athletic pubalgia or osteitis pubis. Rather, it is a spectrum of lesions that are difficult to distinguish clinically from each other.
The abdominal muscle complex consists of the rectus abdominis, the internal oblique, and the external oblique. The function of the rectus abdominis is to bend the spine. The internal and external obliques work together to assist in rotational movements of the trunk. These muscles can be injured during a sudden muscle contraction, or in a sudden twisting in an uncoordinated manner.
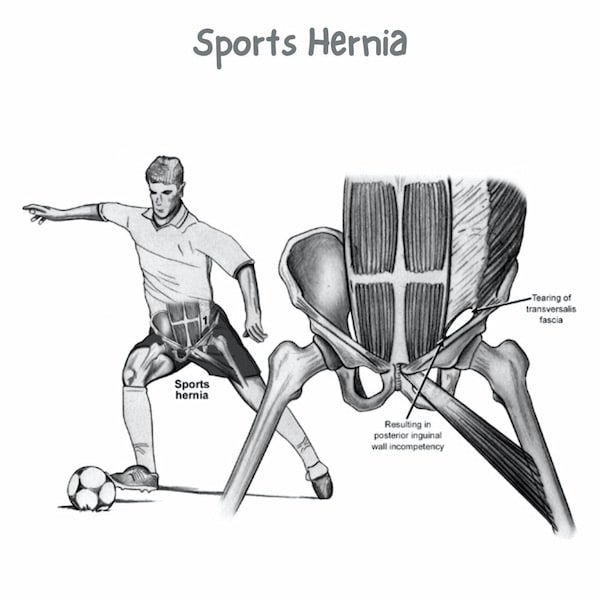

This is a difficult diagnosis. The condition is common in athletes who use the abdominal and core thigh muscle groups a lot, such as football and hockey players.
Symptoms & diagnosis
The athlete is often in pain for a long time before complaining of severe pain to the team staff. The rectus abdominis is most often involved, and the pain is localized at the rectus insertion at the pubic symphysis. Clinical examination and imaging (MRI) often lead to nonspecific findings. The differential diagnosis may include adductor strain, stress fractures, or hip impingement syndrome.
Treatment
The initial treatment includes rest, massage, stretching. This is followed by strengthening and a gradual return to training and play. Mesh surgery is a solution for resistant cases.
Hamstring injuries
The hamstrings are the muscles at the back of the thigh. These muscles are the biceps femoris, semitendinosus and semimembranosus. The hamstrings cause knee flexion and hip extension.

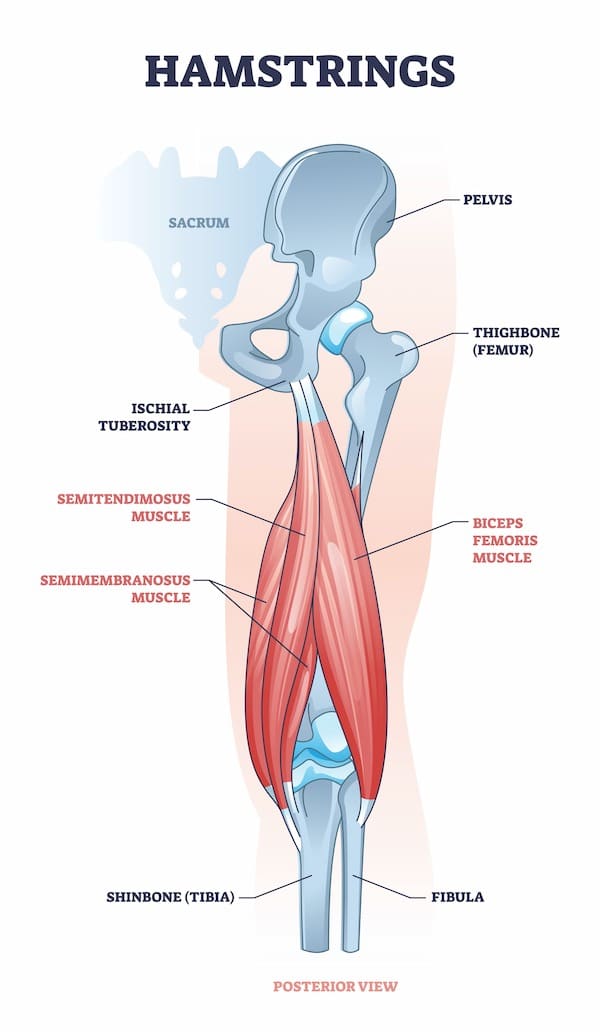
What causes a hamstring injury?
A hamstring injury often occurs during sudden, powerful movements, such as an explosive sprint, or jumps that overstretch the tendons and cause a sudden contraction. The injury can also occur gradually during slower movements.
Repetitive injury is common in athletes. You are more likely to injure your hamstring if you have injured it in the past. Doing regular stretching and strengthening exercises and warming up before exercise can help reduce your risk of hamstring injury.
How do I know I have a hamstring strain?
Mild injuries (grade 1), usually cause sudden pain and tenderness in the back of the thigh. It may be painful to move your leg, but muscle strength will not be affected. Partial hamstring tears (grade 2) are usually more painful. There may also be swelling or bruising in the back of the thigh, as well as loss of muscle strength. Severe hamstring tears (grade 3) are usually very painful, tender, with swelling and ecchymosis, making walking and standing difficult. There may have been a "cracking" sensation at the time of the injury, and you will not be able to use the affected leg.
What's the treatment?
The initial treatment includes rest, massage, stretching. This is followed by strengthening and a gradual return to training and play. Surgery is very rarely needed.
Achilles tendinopathy
The Achilles tendon is the largest and strongest tendon in the human body. The Achilles tendon connects the calf muscles to the heel bone. It is responsible for propulsion when we walk, run or jump. Achilles tendonitis is one of the most common causes of foot and heel pain.


Causes
The condition occurs most often in runners and athletes who participate in sports that require jumping, spinning, or sudden changes of direction, such as basketball, tennis, or soccer. Overuse is the most common cause of Achilles tendonitis. The tendon is subjected to repeated stress or tension, and can develop swelling and inflammation.
Symptoms
Common symptoms include:
- Pain and stiffness, exacerbated by activity
- Swelling of the achilles tendon
- Creaking sensation during movement in the ankle
- Swelling or thickening in the Achilles tendon near the heel
Treatment
The initial treatment is conservative and includes rest, ice therapy, elevation, physical therapy, special insoles, shockwave therapy, etc. Surgical treatment is applied in resistant cases.
FAQs - Frequently Asked Questions
What are the hamstrings?
The hamstrings are the muscles at the back of the thigh:
– Biceps femoris
– Semitendinosus
– Semimembranosus
What are the adductors?
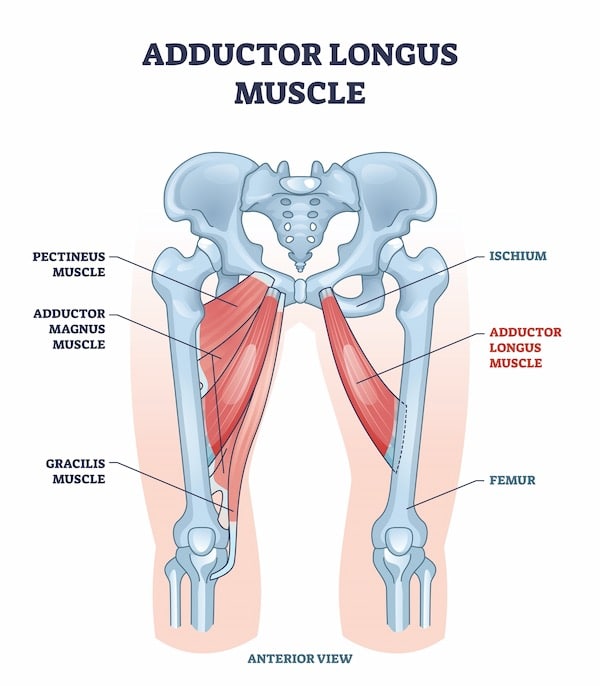
The adductors are the 5 muscles comprising the medial compartment of the thigh:
– Adductor brevis
– Adductor longus
– Adductor magnus
– Gracilis
– Pectineus
Find us
Book an appointment with us today

